The American Diabetes Association recently shared an updated position statement on the management of type 1 diabetes in children and Adolescents. This statement is an update to their previous position statement issued in 2005. Their statement highlights the common sense idea that children are not just mini-adults. Treatment plans for children with Type 1 diabetes need to be tailored to both their current situation and their future growth and development.
The following areas were highlighted in the updated statement of recommendations for children and adolescents with Type 1 Diabetes (T1D):
- Diagnosis of Diabetes
- Blood Glucose Level Management
- Lifestyle Considerations
- Self-Management of Diabetes
- Complications and Comorbidities
- The Transition from Childhood to Adolescence and Adulthood
New Recommendations for Blood Glucose (BG) Management in Children and Adolescents
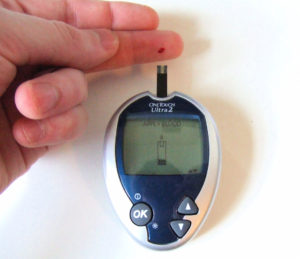
Most children’s T1D should be treated with insulin regimens with either multiple daily injections or via insulin pump therapy. Healthcare professionals should measure A1C levels of their non-adult patients at 3 month intervals. The target level of A1C should be 7.5 %. Patients or their caregivers should monitor BG levels multiple times a day, typically 6 to 10 times.
Medical devices such as insulin pumps and continuous glucose monitors (CGM) can be very helpful in the management of T1D. The ADA recommends that the CGM be considered in all children and adolescents, even though not using insulin pump therapy. Studies have found that compliant use such devices correlates with better BG control, lower A1C levels and reduction in hypoglycemic events.
Adjunctive Therapies for Children with T1D
One highlight in their recommendations between the management of type 1 diabetes in children versus adults is in regard to adjunctive therapies. They do not recommend the use of adjunctive therapies, such as the medication metformin in children. Clinical trials showed that despite the advantages of such therapies to help with weight loss or other diabetes comorbidities, there are more risks than benefits for children.
Check back next month for our follow-up blog talking about the unique behavioral aspects of managing diabetes in children and adolescents. We’ll focus on the challenges of self-management of their disease and other related health and wellness concerns.
Additional Resources
411 on CGM
Exercise for Children with Diabetes
ADA Position Statement













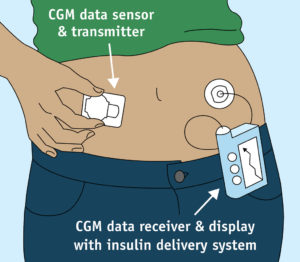 The medical device market is always advancing technologically, as with most other industries. One new technological development, the Continuous Glucose Monitor (CGM), provides added peace of mind to diabetics by providing 24-7 information about blood sugar levels. This constant feedback provided by the device allows for better short and long term control of your diabetes, which will also improve your A1C levels.
The medical device market is always advancing technologically, as with most other industries. One new technological development, the Continuous Glucose Monitor (CGM), provides added peace of mind to diabetics by providing 24-7 information about blood sugar levels. This constant feedback provided by the device allows for better short and long term control of your diabetes, which will also improve your A1C levels.









