Even when you and your family are doing all the right things to avoid illness you can still be unlucky and catch whatever is ‘going around.’ This time of year that means the flu. The 2019 – 2020 flu season has been quite severe with an estimated 31 million people sickened by the virus. More than 14,000 people have died, including almost 100 children.
Monitor Blood Glucose (BG) Levels
The body’s natural reaction to infection will effect blood glucose levels and control. When your child is sick, their routines are disrupted including their eating schedule and appetite which can further impact BG levels. Flu symptoms such as high fevers and sore throats can lead to dehydration and difficulty eating and drinking. The bottom line is that it may be much harder to control BG levels.
- Consider monitoring BG and ketones more frequently while your child is sick
- Maintain normal medication schedules
- Keep normal eating schedules if possible and offer alternatives
- Stay hydrated – adequate fluid will flush excess ketones and prevent dehydration that can raise BG levels.
- Focus on carb-free and caffeine free beverages to minimize impact on BG levels

Beware of Over- the-counter Medications (OTC) for Cold and Flu Symptoms
- Check ingredients: Cough syrup may contain added sugar that can worsen BG control. Look for medications in pill form or sugar free options.
- Educate yourself about medication side effects: Acetaminophen may cause false readings on a CGM, Ibuprofen and aspirin can lower BG levels by interfering with the insulin metabolism. Decongestants like pseudo epinephrine can raise BG levels.
- Ask for guidance: Check with your healthcare provider for recommendations on OTC cold and flu medications.
- Consider non-drug treatment options first: These include fluids, cold compresses, humidifiers, and saline sprays and rinses.
Diabetic Ketoacidosis (DKA)
DKA is an acute complication that can occur in T1 diabetics when their body shifts from using glucose for fuel to ketones – which are derived from fatty acids. Children with the flu may be at higher risk for this serious condition.
Know When to Call your Healthcare Provider
Just like anyone else, children with T1D may need to see their healthcare provider when flu or cold symptoms worsen.
- Fever over 103 degrees or a fever that lingers for days without other symptoms.
- High BG levels and/or ketones in your urine – based on recommendation from your healthcare provider.
- Inability to keep food or liquid down, severe vomiting or diarrhea, decreased urination or other signs of dehydration. Lack of interest in eating or drinking.
- Difficulty breathing or blue lips.
If you think your child may have the flu your healthcare provider can test for it and prescribe antiviral medication. These drugs won’t cure the flu but may reduce the severity of the illness.
Additional Resources:
Recommendations from the CDC – Flu and People with Diabetes
Type 1 Diabetes Recommendations from the American Diabetes Association (ADA)
Tips for Managing Type 1 Diabetes at School
















 Fight Stress – Have your whole family learn a new technique to relieve stress such as yoga, mindfulness, or mediation. Parents need to practice what they preach!
Fight Stress – Have your whole family learn a new technique to relieve stress such as yoga, mindfulness, or mediation. Parents need to practice what they preach!


 For many years, researchers have theorized that type 1 diabetes is an autoimmune disorder, where the body attacks healthy insulin producing cells in the body instead of bacteria and viruses. However, the exact reason why the autoimmune response occurs had not been discovered.
For many years, researchers have theorized that type 1 diabetes is an autoimmune disorder, where the body attacks healthy insulin producing cells in the body instead of bacteria and viruses. However, the exact reason why the autoimmune response occurs had not been discovered.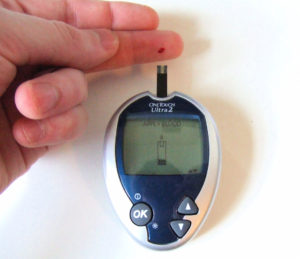 Hypoglycemia unawareness is a complication of T1D where the patient misses the typical symptoms of a blood sugar drop (palpitations, sweating, anxiety, etc.). When their body does not release adrenaline there are no warning symptoms and then they are at risk for life threatening complications.
Hypoglycemia unawareness is a complication of T1D where the patient misses the typical symptoms of a blood sugar drop (palpitations, sweating, anxiety, etc.). When their body does not release adrenaline there are no warning symptoms and then they are at risk for life threatening complications.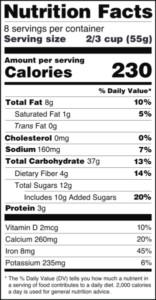
 Children with diabetes already need to monitor their food intake to manage their condition. By moving focus away from processed foods with lots of added sugar to whole foods like fruits, vegetables and dairy items, children will get better nutrition. Whole foods with naturally occurring sugars also provide vitamins, minerals, fiber and antioxidants instead of empty calories.
Children with diabetes already need to monitor their food intake to manage their condition. By moving focus away from processed foods with lots of added sugar to whole foods like fruits, vegetables and dairy items, children will get better nutrition. Whole foods with naturally occurring sugars also provide vitamins, minerals, fiber and antioxidants instead of empty calories. 
 The year has flown by and Thanksgiving is only a few weeks away. For many, this holiday means overindulgence. For diabetics, it can be a very difficult time for many reasons. The hardest is resisting temptations. Who doesn’t love seconds or even thirds of their favorite dishes; i.e., mashed potatoes? An important thing to remember is “everything in moderation.” Here are a few tips to budget your calories and manage your blood sugar while still enjoying this wonderful time with family.
The year has flown by and Thanksgiving is only a few weeks away. For many, this holiday means overindulgence. For diabetics, it can be a very difficult time for many reasons. The hardest is resisting temptations. Who doesn’t love seconds or even thirds of their favorite dishes; i.e., mashed potatoes? An important thing to remember is “everything in moderation.” Here are a few tips to budget your calories and manage your blood sugar while still enjoying this wonderful time with family. The number of Americans that suffer from depression, also known as Major Depressive Disorder is increasing all the time. Depression is more than being sad or in a bad mood. This condition is a chemical imbalance in the brain.
The number of Americans that suffer from depression, also known as Major Depressive Disorder is increasing all the time. Depression is more than being sad or in a bad mood. This condition is a chemical imbalance in the brain.  As a diabetic patient or parent, you are well aware that you need an emergency diabetes bag. This is one project that can’t be put off.
As a diabetic patient or parent, you are well aware that you need an emergency diabetes bag. This is one project that can’t be put off.









