
Have you or your family made any New Year’s resolutions this year? Often times resolutions focus on our health. If limiting snacks or just eating a healthier diet is among your family’s New Year’s resolutions you might wonder about the impact of media on our food choices – both good and bad. Cooking shows are very popular and can focus on a type of cuisine, baking, or even tips for streamlining your family’s meal preparation.
A recent study from the Journal of Nutritional Education and Behavior gives new insight into how television cooking shows influence the eating habits of children.
Study Details
- 125 children ages 10 to 12 from the Netherlands
- Study participants viewed a ten minute child-oriented cooking program
- The study was conducted in a school environment
- Study participants were offered a snack to thank them for participating
- Snack offerings included healthy options such as apples and cucumbers as well as less healthy options such as chips and pretzels.
Study Findings
It is not surprising that some of the children who watched the cooking segment featuring healthy food options chose to eat a healthy snack. What is compelling is the magnitude of the effect.
Children shown the program featuring food preparation with healthy options were 2.7 times more likely to pick a healthy snack as a reward versus those who watched a program featuring unhealthy foods.
Study authors also noted that the cooking programs provided exposure to new healthy food options to children and their families. The cooking shows modeled portion control and showcased healthier food options in a positive light.
Make Healthy Eating a Family Activity
Research has shown that children are more likely to eat (or at least try) fruits and vegetables if they help prepare them. Cooking healthy meals for your family will require more preparation. Remember to involve your children in grocery shopping and meal planning too!
Poor dietary choices in childhood and adolescence can negatively impact health for a lifetime. Selecting healthy food options help our families maintain healthy weights and minimize the risk of diseases related to obesity.
Just like good food choices, remember to make good media choices for your family, for better health in the New Year and beyond.
Additional Resources:
Journal of Nutrition Education and Behavior Study
Using a Low Carb Diet to Help Treat Type 1 Diabetes
Added Sugar Amounts Now on Nutrition Facts Panel















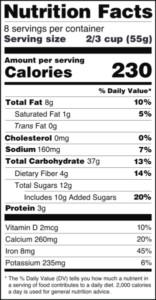
 Children with diabetes already need to monitor their food intake to manage their condition. By moving focus away from processed foods with lots of added sugar to whole foods like fruits, vegetables and dairy items, children will get better nutrition. Whole foods with naturally occurring sugars also provide vitamins, minerals, fiber and antioxidants instead of empty calories.
Children with diabetes already need to monitor their food intake to manage their condition. By moving focus away from processed foods with lots of added sugar to whole foods like fruits, vegetables and dairy items, children will get better nutrition. Whole foods with naturally occurring sugars also provide vitamins, minerals, fiber and antioxidants instead of empty calories. 
 Over the last two decades, asthma and obesity have reached epidemic proportions. Obesity is a common comorbidity to asthma and it is commonly thought that obesity precedes the asthma symptoms. Now, the question has been raised about whether it is the other way around. Does obesity follow on the heels of asthma or is it asthma that raises the likelihood of becoming overweight?
Over the last two decades, asthma and obesity have reached epidemic proportions. Obesity is a common comorbidity to asthma and it is commonly thought that obesity precedes the asthma symptoms. Now, the question has been raised about whether it is the other way around. Does obesity follow on the heels of asthma or is it asthma that raises the likelihood of becoming overweight?
 I have often thought that there has to be ways to boost my body’s ability to care for itself without adding to my medicine cabinet. There has been a surge in patients seeking naturopathic doctors, as well as traditional medical doctors researching the benefits of naturopathic remedies alongside necessary prescriptions. Many clinical trials have shown that herbs can successfully assist in the treatment of various diseases such as diabetes. The traditional medical system of India, Ayurvedic medicine, finds the following herbs to help manage diabetes. It is still extremely important to maintain your relationship with your doctor and to check in before trying any herbal supplements. However, herbs can become a complimentary support to your regular treatment plan.
I have often thought that there has to be ways to boost my body’s ability to care for itself without adding to my medicine cabinet. There has been a surge in patients seeking naturopathic doctors, as well as traditional medical doctors researching the benefits of naturopathic remedies alongside necessary prescriptions. Many clinical trials have shown that herbs can successfully assist in the treatment of various diseases such as diabetes. The traditional medical system of India, Ayurvedic medicine, finds the following herbs to help manage diabetes. It is still extremely important to maintain your relationship with your doctor and to check in before trying any herbal supplements. However, herbs can become a complimentary support to your regular treatment plan. 
 With the advent of apps for smartphones, there’s something nostalgic about using a pen and paper. At meetings, I often find myself still jotting down action items in a notebook instead of in my iPad. But, when it comes to tracking my health, I’m grateful to have so many intuitive and user-friendly apps at my disposal. I can track my sleep habits, exercise and diet easily with my smartphone. There are also a number of useful health tracking apps available for individuals with specific conditions like asthma and diabetes.
With the advent of apps for smartphones, there’s something nostalgic about using a pen and paper. At meetings, I often find myself still jotting down action items in a notebook instead of in my iPad. But, when it comes to tracking my health, I’m grateful to have so many intuitive and user-friendly apps at my disposal. I can track my sleep habits, exercise and diet easily with my smartphone. There are also a number of useful health tracking apps available for individuals with specific conditions like asthma and diabetes.

 When we get hurt or have an infection, the body’s natural response is to trigger inflammation. Short-term inflammation helps the body heal as white blood cells fight off bacteria and viruses. Normal inflammation
When we get hurt or have an infection, the body’s natural response is to trigger inflammation. Short-term inflammation helps the body heal as white blood cells fight off bacteria and viruses. Normal inflammation  The media often focuses on the rising risk of type 2 diabetes on a regular basis, and the importance of diet and exercise as ways to prevent against the disease. A
The media often focuses on the rising risk of type 2 diabetes on a regular basis, and the importance of diet and exercise as ways to prevent against the disease. A  Eating healthy isn’t just good for your waistline, a new study shows that children with asthma can experience reduced symptoms by avoiding certain fatty foods and incorporating omega-3 fish oils to their diet. Asthma is the top reason children miss school, and obese children don’t respond as well to their asthma medicine. Dr. Jason Lang, a Pulmonary Pediatrician at Nemours Children’s Hospital, is conducting the
Eating healthy isn’t just good for your waistline, a new study shows that children with asthma can experience reduced symptoms by avoiding certain fatty foods and incorporating omega-3 fish oils to their diet. Asthma is the top reason children miss school, and obese children don’t respond as well to their asthma medicine. Dr. Jason Lang, a Pulmonary Pediatrician at Nemours Children’s Hospital, is conducting the 









