 An incredible amount of research has gone into childhood asthma in the last few years, leading to deeper understanding of the condition and better care for children with asthma.
An incredible amount of research has gone into childhood asthma in the last few years, leading to deeper understanding of the condition and better care for children with asthma.
New technology hopes to help predict a child’s asthma attacks before they occur. A wearable asthma informatics system is under development as part of an initiative of the US National Institutes of Health.
What is PRISMS?
This new asthma monitoring system is part of the PRISMS Initiative, which stands for Pediatric Research Using Integrated Sensor Monitoring Systems. A team of researchers from University of California-Los Angeles and the University of Southern California are developing an integrated platform of wearable sensors that can gather data about the environment of children with asthma and help predict asthma attacks.
How does the Asthma Informatics Platform Work?
The platform connects a variety of sensors and equipment using bluetooth and wi-fi, compiling all the data for health professionals. The platform includes the following:
Smart Watch: acts as a hub connecting to all other devices during the day and collects bioinformatics like activity level and heart rate.
Air Quality Sensor: attached to backpack or placed nearby and measures very small particulates in the air that can make asthma worse.
Medication Sensor: receptor in inhaler that records when medicine is taken.
Spirometer: measures the volume of breath twice a day, data is automatically sent to the system.
Smartphone app: includes questionnaires to gather data from the child about their environment.
How will PRISMS help asthma care?
With the data that PRISMS collects, medical professionals can identify patterns and help families identify asthma triggers. In the future, a platform like PRISMS could send alerts when sensors detect that an asthma attack is likely.
Overall, using the data from all children in the study, researchers hope to find new trends in childhood asthma. Patterns realized from the data of the children in the study may lead to new treatments and new environmental policies to keep all children healthy.
New Technology will bring better care for children with Asthma
In the future, portable medical health devices may be commonplace, and the data collected from systems like PRISMS will help make asthma care better than ever.
Resources
Predicting Asthma Attacks in Kids – Chemical & Engineering News
PRISMS Initiative – National Institutes of Health
Got Asthma or Allergies? There’s an App for That!













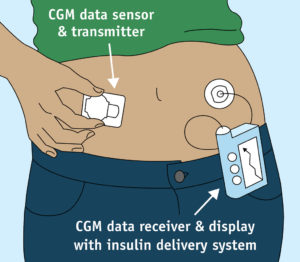 The medical device market is always advancing technologically, as with most other industries. One new technological development, the Continuous Glucose Monitor (CGM), provides added peace of mind to diabetics by providing 24-7 information about blood sugar levels. This constant feedback provided by the device allows for better short and long term control of your diabetes, which will also improve your A1C levels.
The medical device market is always advancing technologically, as with most other industries. One new technological development, the Continuous Glucose Monitor (CGM), provides added peace of mind to diabetics by providing 24-7 information about blood sugar levels. This constant feedback provided by the device allows for better short and long term control of your diabetes, which will also improve your A1C levels.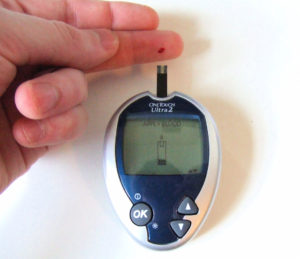 If you have Type 1 diabetes, your entire day can be spent treating your condition. Over the past few decades, technology has advanced significantly, making life as a Type 1 diabetic easier than ever before. The FDA approval of a new medical device called the artificial pancreas in September 2016 will continue this trend. Derek Rapp, President and CEO for the
If you have Type 1 diabetes, your entire day can be spent treating your condition. Over the past few decades, technology has advanced significantly, making life as a Type 1 diabetic easier than ever before. The FDA approval of a new medical device called the artificial pancreas in September 2016 will continue this trend. Derek Rapp, President and CEO for the  With the advent of apps for smartphones, there’s something nostalgic about using a pen and paper. At meetings, I often find myself still jotting down action items in a notebook instead of in my iPad. But, when it comes to tracking my health, I’m grateful to have so many intuitive and user-friendly apps at my disposal. I can track my sleep habits, exercise and diet easily with my smartphone. There are also a number of useful health tracking apps available for individuals with specific conditions like asthma and diabetes.
With the advent of apps for smartphones, there’s something nostalgic about using a pen and paper. At meetings, I often find myself still jotting down action items in a notebook instead of in my iPad. But, when it comes to tracking my health, I’m grateful to have so many intuitive and user-friendly apps at my disposal. I can track my sleep habits, exercise and diet easily with my smartphone. There are also a number of useful health tracking apps available for individuals with specific conditions like asthma and diabetes.












