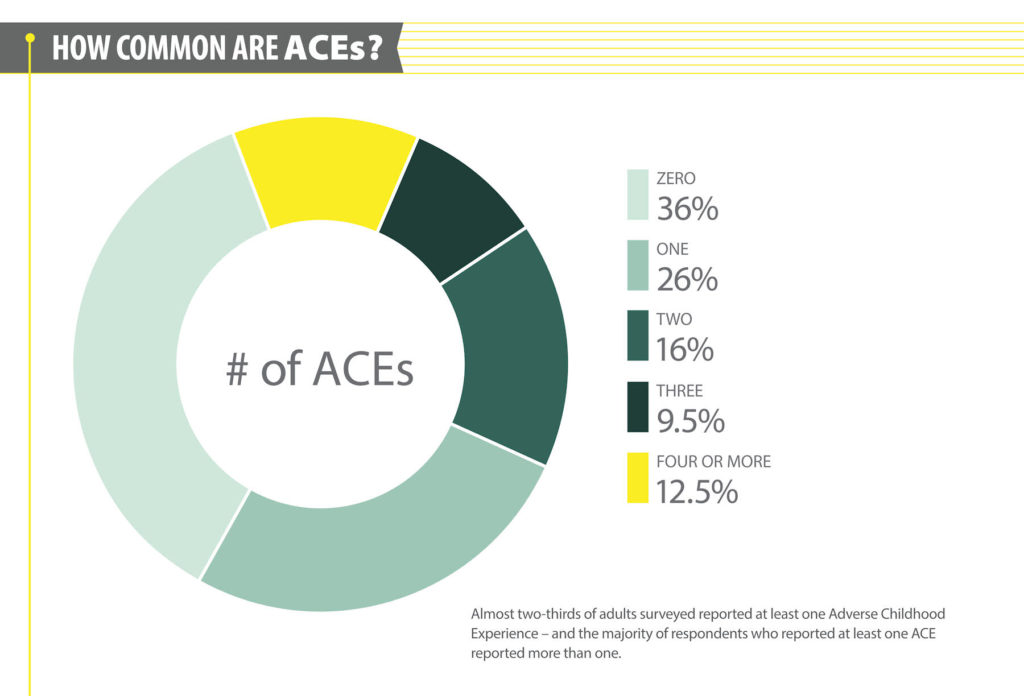
The CDC’s Adverse Childhood Events Study (ACE study) revealed a remarkable connection between traumatic events in childhood and chronic diseases and social and emotional problems in adulthood. High ACE scores may mean significantly higher rates of heart disease, lung cancer, diabetes, depression and risk of suicide.
As you would expect, the higher your ACE score, the higher your risk of health issues in adulthood. Studies show with an ACE score of 4 or more your risk of a host of chronic health conditions increases by over 200%. Specifically the risk of depression increases by 400%; the risk of suicide by 1000%. Nearly two-thirds of adults have at least one ACE.
Staggering Statistics
- An ACE score of 4 increases your odds of getting asthma by 73%
- A traumatic event during childhood (just one ACE) can triple the risk of developing Type 1 diabetes.
Does a high ACE score sentence you to a life filled with chronic disease?
Pediatrician Nadine Burke Harris believes the answer to that question is a resounding NO. She has personally seen the positive impact of interventional programs where healthcare providers and community resources work together to support those at risk.
Dr. Harris’ approach suggests the following:
- Screen all patients routinely to determine ACE scores.
- Provide additional support to families with children with high ACE scores including home visits from professionals, mental health care, nutrition counseling, holistic interventions, and if needed, medications.
- Educate parents on the negative impacts of chronic stress
- Increase treatment for patients with asthma or diabetics with higher ACEs scores.
Resilience and Children with Chronic Diseases
Can we train our brains to be more resilient in the face of personal struggles and health problems? Here are a few tips on how to help your child be more resilient.
Focus on the positive – Encourage your child to connect with friends and other adults. Support activities and hobbies where your child can build relationships with those with similar interests and build confidence.
Banish Blame –Children may feel guilty that they have a chronic illness. Empower them to live their best life and work through their chronic disease’s challenges.
 Fight Stress – Have your whole family learn a new technique to relieve stress such as yoga, mindfulness, or mediation. Parents need to practice what they preach!
Fight Stress – Have your whole family learn a new technique to relieve stress such as yoga, mindfulness, or mediation. Parents need to practice what they preach!
Validate Emotions – Children may have difficulty verbalizing what they are feeling. Listen first and always acknowledge their feelings.
Remain Optimistic – Life is a journey and your child and family may experience setbacks. Help your child set and strive for realistic goals.
Hug Often – Don’t underestimate the value of a hug as a tangible reminder of your love and support. Research shows that giving and receiving hugs reduces stress, and has a host of health related benefits.
We’re All in This Together
ACEs affect all of us directly or indirectly regardless of income level, and impact lifelong health and social well-being. Together, we can lessen these effects by teaching and learning resilience skills, and adopting trauma-informed practices and policies.
Check out some of the resources below for more information about ACE and how to build resilience to combat the effects of chronic stress.
Additional Resources
CDC ACE Study Website
How Childhood Trauma Affects Health Across a Lifetime – Ted Talk by Nadine Burke Harris, MD.
ACE Connections Blog
ACEs Quiz link
Six Skills to Help Build Resilience (narrated)
Building Resilience in Children
Wake County NC Resilience Initiative
Benefits of the 20 Second Hug















 The NC Department of Health and Human Services released new figures about the
The NC Department of Health and Human Services released new figures about the 









