 Telehealth has been around for a while, but during the COVID-19 pandemic its use grew dramatically. COVID-19 has made many of us consider telehealth visits vs in-person ones. For some practitioners that was the only way they saw patients during the pandemic. This healthcare delivery method has advantages for both the practitioner and patient.
Telehealth has been around for a while, but during the COVID-19 pandemic its use grew dramatically. COVID-19 has made many of us consider telehealth visits vs in-person ones. For some practitioners that was the only way they saw patients during the pandemic. This healthcare delivery method has advantages for both the practitioner and patient.
Recent studies from the National Institutes of Health showed that 30% of outpatient visits during the pandemic utilized telehealth. While overall medical visits were down, the use of telehealth increased 23 times when comparing months prior and during the COVID-19 pandemic period that began in March 2020.
Telehealth visit advantages:
● Scheduling convenience – less time missed from school or work
● Patients may miss fewer appointments
● Lower costs – telehealth visits are cost effective for families
● Expanded options – visits to out of town specialists are possible without travel
● Increased efficiencies – telehealth visits can allow more time for patient education
● Reduced risk of infection – online visits limit exposure to others and potential contagions in the healthcare practitioners office
Telehealth visit challenges:
● Technology is required for both the patient and practitioner for a successful telehealth appointment including high speed internet connections and web cameras or smart phones.
● Some patients may not be comfortable meeting with healthcare provider over the internet.
What should families consider in choosing between in-person vs telehealth visits?
While telehealth visits can work for an acute infection like strep throat they won’t always be appropriate for asthma patients.
Here are a few scenarios to consider a telehealth appointment for your asthma management:
● Prescription refills for your asthma medications
● Routine follow-up appointments when your symptoms are under control
● New or increased asthma or allergy symptoms that are under control
● Review mild medication side effects
● Asthma education needs like how to use equipment (inhalers, nebulizers) or your medications
However, if you need a test or if your provider needs to check vital signs or breathing, you will likely need to schedule an in-person visit. Examples of a reason for on in-person visit would include new or worsening symptoms that require increased use of a rescue inhaler.
Bottom line – out of control asthma symptoms needs urgent in-person follow-up!
Just like with any regular medical appointment remember to get organized prior to your visit:
● Prepare a list of questions for your healthcare provider
● Confirm what your insurance plan covers in terms of telehealth and any associated costs
● Check out your internet connectivity and test any portal logins prior to the appointment
Telehealth healthcare visits give patients more options to keep their asthma in control and manage symptoms. Check out if your provider uses telehealth and save some time and money on your next visit.
Additional Resources:
National Institutes of Health article: Patient satisfaction with telemedicine encounters in an allergy and immunology practice during the coronavirus disease 2019 pandemic
Centers for Disease Control article: Using Telehealth to Expand Access to Essential Health Services during the COVID-19 Pandemic
Hidden Spots for Germs: Home, Office and Doctor’s Office













 Vitamin C is a well-known immunity boosting food. This vitamin is thought to increase the production of white blood cells, which are key to fighting infections in the body.
Vitamin C is a well-known immunity boosting food. This vitamin is thought to increase the production of white blood cells, which are key to fighting infections in the body.  Ginger is a well-known natural remedy for nausea. The flavorful root contains gingerol – a relative of capsaicin found in spicy peppers which may help reduce inflammation in our bodies.
Ginger is a well-known natural remedy for nausea. The flavorful root contains gingerol – a relative of capsaicin found in spicy peppers which may help reduce inflammation in our bodies. Reduce Screen Time – Yes that means your phone too!
Reduce Screen Time – Yes that means your phone too! Lead with information not accusations. If you suspect your teen is vaping or might have friends who are, start with the facts and your concerns versus putting them on the spot with a direct question like, “Are you vaping?”
Lead with information not accusations. If you suspect your teen is vaping or might have friends who are, start with the facts and your concerns versus putting them on the spot with a direct question like, “Are you vaping?”

 Fight Stress – Have your whole family learn a new technique to relieve stress such as yoga, mindfulness, or mediation. Parents need to practice what they preach!
Fight Stress – Have your whole family learn a new technique to relieve stress such as yoga, mindfulness, or mediation. Parents need to practice what they preach! An incredible amount of research has gone into childhood asthma in the last few years, leading to deeper understanding of the condition and better care for children with asthma.
An incredible amount of research has gone into childhood asthma in the last few years, leading to deeper understanding of the condition and better care for children with asthma. It’s that time of year again. A fun summer has come and gone and it’s time to start thinking about back to school. While stocking up on school supplies, don’t forget to prepare your child’s asthma plan for the new school year.
It’s that time of year again. A fun summer has come and gone and it’s time to start thinking about back to school. While stocking up on school supplies, don’t forget to prepare your child’s asthma plan for the new school year. No one should be inhaling any of these toxic substances because they will all cause inflammation in your lungs. Asthma sufferers and those with allergies are especially at risk of exposure to lung irritants. Studies by the National Academies of Science indicate that e-cigarette use increases asthma symptoms such as coughing and wheezing.
No one should be inhaling any of these toxic substances because they will all cause inflammation in your lungs. Asthma sufferers and those with allergies are especially at risk of exposure to lung irritants. Studies by the National Academies of Science indicate that e-cigarette use increases asthma symptoms such as coughing and wheezing. The statistics on the rates of vaping are staggering. In 2018 the CDC reported that 20% of high school students vaped in the past 30 days. Smoking rates in the same age group are actually lower at only 8 percent. The rate of teen smoking continues to fall; it is 50% lower than it was in 2011.
The statistics on the rates of vaping are staggering. In 2018 the CDC reported that 20% of high school students vaped in the past 30 days. Smoking rates in the same age group are actually lower at only 8 percent. The rate of teen smoking continues to fall; it is 50% lower than it was in 2011.
 Well controlled asthma means that your child is in the GREEN zone of the asthma action plan. Good control implies that your child’s symptoms such as coughing, wheezing or shortness of breath occur only two or fewer days per week.
Well controlled asthma means that your child is in the GREEN zone of the asthma action plan. Good control implies that your child’s symptoms such as coughing, wheezing or shortness of breath occur only two or fewer days per week. 
 We hear all the time from multiple sources to get more exercise. Everyone has their reasons for not getting enough. We all know we should do it more, but feel like we don’t have enough time or energy to do so. If you suffer from asthma, you may fear that working out would make your symptoms worse. Here are some of the best options for exercising with asthma
We hear all the time from multiple sources to get more exercise. Everyone has their reasons for not getting enough. We all know we should do it more, but feel like we don’t have enough time or energy to do so. If you suffer from asthma, you may fear that working out would make your symptoms worse. Here are some of the best options for exercising with asthma Asthma is a challenging, but very treatable illness. There are many medications and tools available to help relieve symptoms. Did you know that asthma prevention can start in your kitchen? Not all foods are created equal. What foods might be best for asthmatics? There are even healthy foods that may worsen your asthma symptoms.
Asthma is a challenging, but very treatable illness. There are many medications and tools available to help relieve symptoms. Did you know that asthma prevention can start in your kitchen? Not all foods are created equal. What foods might be best for asthmatics? There are even healthy foods that may worsen your asthma symptoms. Music is a wonderful stress release for many people. For some, the release comes from listening to the music and relating to the lyrics. It strikes a chord inside of us all. For others, making music is the release. Whether you play an instrument or sing, you are successfully dissolving the stress of your day-to-day. Congratulations! You have found an outlet.
Music is a wonderful stress release for many people. For some, the release comes from listening to the music and relating to the lyrics. It strikes a chord inside of us all. For others, making music is the release. Whether you play an instrument or sing, you are successfully dissolving the stress of your day-to-day. Congratulations! You have found an outlet. Summer is coming to a close for students in North Carolina. The change of seasons and environment can spell trouble for asthma and allergy sufferers. They already know their at-home triggers and how to combat them, but have less control over their environment at school. Common classroom triggers include pollen, dust mites, mold, chalk dust, and pet dander. With the help of school administrators and parents, students can remain focused on their studies and less on their allergies.
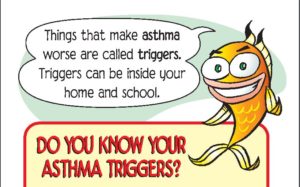
Summer is coming to a close for students in North Carolina. The change of seasons and environment can spell trouble for asthma and allergy sufferers. They already know their at-home triggers and how to combat them, but have less control over their environment at school. Common classroom triggers include pollen, dust mites, mold, chalk dust, and pet dander. With the help of school administrators and parents, students can remain focused on their studies and less on their allergies.










