 The number of Americans that suffer from depression, also known as Major Depressive Disorder is increasing all the time. Depression is more than being sad or in a bad mood. This condition is a chemical imbalance in the brain.
The number of Americans that suffer from depression, also known as Major Depressive Disorder is increasing all the time. Depression is more than being sad or in a bad mood. This condition is a chemical imbalance in the brain.
Unfortunately, depression often goes undiagnosed and, therefore, untreated. As it turns out, diabetics are especially vulnerable to this condition.
Diabetics At Double the Risk of Depression
Several studies have found that diabetics are at double the risk of suffering from depression due to the physical and emotional stress of their chronic disease. A depressed diabetic is more likely to neglect his/her diet or medication plan, which is critical to their well-being. The cause is unclear, however if a patient’s depression is stress induced, a diabetic may be a greater risk because of a metabolic imbalance that already exists.
Managing a chronic condition like diabetes can be overwhelming, leaving less time and energy for dealing with life’s other challenges. The financial burden of treating diabetes may also be a contributing factor to higher rates of depression. The rising medical costs of their life sustaining treatment adds another burden.
Studies also suggest that diabetics who have a history of depression are at a higher risk of developing diabetic complications than those without. This is because depressed individuals have elevated levels of stress hormones such as cortisol, which can affect blood sugar metabolism and increase insulin resistance.
What to Watch for: Symptoms of Depression
People suffering from depression may not want to get out of bed in the morning. They neglect their diet and don’t exercise. Depressed people shun social gatherings and have trouble staying motivated at work or school.
Seek help if you are experiencing any of the following symptoms:
• Difficulty concentrating, forgetfulness and poor decision making
• Feelings of guilt, worthlessness and/or helplessness
• Insomnia or excessive sleep
• Irritability or restlessness
• Loss of interest in activities once enjoyed
• Overeating or not eating enough (dangerous for diabetics)
• Aches and pains including headaches, cramps, and digestive problems
• Persistent sadness, anxiety, and feelings of emptiness
• Thoughts of suicide or attempting suicide
Depression can be brought on by a number of factors including genetics, life circumstances, trauma, side effects of medication, stress, or other environmental factors. It is treatable with psychotherapy, as well as medication. As with most medications, anti-depressants (often called SSRIs, which stands for Selective Serotonin Reuptake Inhibitor) come with side effects including nausea, weight gain, fatigue, insomnia, dry mouth, dizziness, irritability, and anxiety.
You may have chalked your feelings of sadness up to the fact that you’re diabetic when you may also be depressed. Depression should be treated as a separate condition. Getting treatment for it can help you take better care of your diabetes, putting you in optimal health.
Additional Resources:
http://www.diabetes.org/living-with-diabetes/complications/mental-health/depression.html
https://www.childrensdiabetesfoundation.org/diabetes-and-depression/














 First and foremost, you cannot communicate enough with school staff including teachers, bus drivers, and health personnel about your child’s condition. Provide as much information as possible so they will know how to assist your child when the need arises.
First and foremost, you cannot communicate enough with school staff including teachers, bus drivers, and health personnel about your child’s condition. Provide as much information as possible so they will know how to assist your child when the need arises. As a diabetic patient or parent, you are well aware that you need an emergency diabetes bag. This is one project that can’t be put off.
As a diabetic patient or parent, you are well aware that you need an emergency diabetes bag. This is one project that can’t be put off.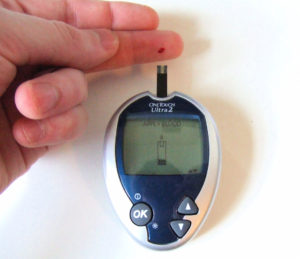 Have you thought about what you would do if your insulin pump were to fail? It is important to have a plan in place for when and if this occurs. You can create a fail-safe plan for the rare event of a pump failure by following these four steps.
Have you thought about what you would do if your insulin pump were to fail? It is important to have a plan in place for when and if this occurs. You can create a fail-safe plan for the rare event of a pump failure by following these four steps. Keep the following items with you at all times, making sure all are within the prescription limits and not expired:
Keep the following items with you at all times, making sure all are within the prescription limits and not expired: If you have diabetes, stress can take a larger toll on your body. When the body is under stress, it acts as if it is under attack. Cortisol (the stress hormone) levels rise, causing your body to store energy in the form of glucose and fat. In diabetics, this process can be disrupted. The glucose is released, and if it can’t be stored, it builds up in your bloodstream.
If you have diabetes, stress can take a larger toll on your body. When the body is under stress, it acts as if it is under attack. Cortisol (the stress hormone) levels rise, causing your body to store energy in the form of glucose and fat. In diabetics, this process can be disrupted. The glucose is released, and if it can’t be stored, it builds up in your bloodstream. Believe it or not, the upcoming travel season is upon us. If you’re diabetic and planning a trip, you may be a bit anxious about how best to manage your condition while away from home. You’re not alone.
Believe it or not, the upcoming travel season is upon us. If you’re diabetic and planning a trip, you may be a bit anxious about how best to manage your condition while away from home. You’re not alone.
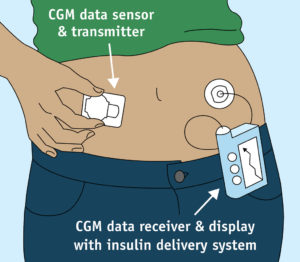 The medical device market is always advancing technologically, as with most other industries. One new technological development, the Continuous Glucose Monitor (CGM), provides added peace of mind to diabetics by providing 24-7 information about blood sugar levels. This constant feedback provided by the device allows for better short and long term control of your diabetes, which will also improve your A1C levels.
The medical device market is always advancing technologically, as with most other industries. One new technological development, the Continuous Glucose Monitor (CGM), provides added peace of mind to diabetics by providing 24-7 information about blood sugar levels. This constant feedback provided by the device allows for better short and long term control of your diabetes, which will also improve your A1C levels.


 I have often thought that there has to be ways to boost my body’s ability to care for itself without adding to my medicine cabinet. There has been a surge in patients seeking naturopathic doctors, as well as traditional medical doctors researching the benefits of naturopathic remedies alongside necessary prescriptions. Many clinical trials have shown that herbs can successfully assist in the treatment of various diseases such as diabetes. The traditional medical system of India, Ayurvedic medicine, finds the following herbs to help manage diabetes. It is still extremely important to maintain your relationship with your doctor and to check in before trying any herbal supplements. However, herbs can become a complimentary support to your regular treatment plan.
I have often thought that there has to be ways to boost my body’s ability to care for itself without adding to my medicine cabinet. There has been a surge in patients seeking naturopathic doctors, as well as traditional medical doctors researching the benefits of naturopathic remedies alongside necessary prescriptions. Many clinical trials have shown that herbs can successfully assist in the treatment of various diseases such as diabetes. The traditional medical system of India, Ayurvedic medicine, finds the following herbs to help manage diabetes. It is still extremely important to maintain your relationship with your doctor and to check in before trying any herbal supplements. However, herbs can become a complimentary support to your regular treatment plan.  With the advent of apps for smartphones, there’s something nostalgic about using a pen and paper. At meetings, I often find myself still jotting down action items in a notebook instead of in my iPad. But, when it comes to tracking my health, I’m grateful to have so many intuitive and user-friendly apps at my disposal. I can track my sleep habits, exercise and diet easily with my smartphone. There are also a number of useful health tracking apps available for individuals with specific conditions like asthma and diabetes.
With the advent of apps for smartphones, there’s something nostalgic about using a pen and paper. At meetings, I often find myself still jotting down action items in a notebook instead of in my iPad. But, when it comes to tracking my health, I’m grateful to have so many intuitive and user-friendly apps at my disposal. I can track my sleep habits, exercise and diet easily with my smartphone. There are also a number of useful health tracking apps available for individuals with specific conditions like asthma and diabetes. The rate of children with type 2 diabetes has declined since 2002, but unfortunately, the
The rate of children with type 2 diabetes has declined since 2002, but unfortunately, the 

 It’s easy to recognize the effects of air pollution on our ability to breathe, but air pollution can cause a myriad of other health conditions. Air pollution is the ninth most important cardiovascular risk factor for
It’s easy to recognize the effects of air pollution on our ability to breathe, but air pollution can cause a myriad of other health conditions. Air pollution is the ninth most important cardiovascular risk factor for 
 Gender plays an interesting role in how diabetes affects those with the condition. For example, pregnant women carrying a baby boy are at a higher risk of developing
Gender plays an interesting role in how diabetes affects those with the condition. For example, pregnant women carrying a baby boy are at a higher risk of developing 









